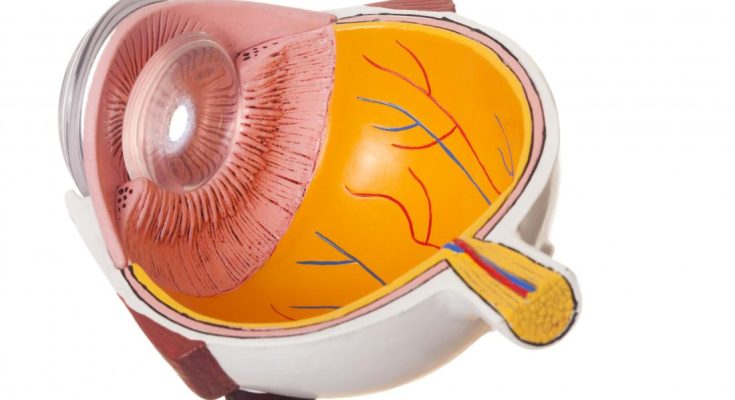
Central serous chorioretinopathy (CSC) is an eye condition that primarily affects the central part of the retina called the macula. It causes a build-up of fluid underneath the retina, leading to blurry or distorted vision. While the condition often resolves on its own in some cases, treatment may be required when symptoms persist or become recurrent. Understanding the long-term vision prognosis after CSC treatment can help patients make informed decisions about managing their eye health and expectations.
Understanding Central Serous Chorioretinopathy
CSC typically affects people between the ages of 30 and 50 and is more common in men than women. It’s often associated with high stress levels, corticosteroid use, or certain systemic conditions. The condition leads to a detachment of the retina due to fluid accumulation, which can distort vision, create blind spots, or reduce visual clarity in the central field.
Most cases of CSC are acute and may resolve spontaneously within three to four months. However, chronic or recurrent cases may require medical intervention. Understanding how treatment affects long-term outcomes is crucial, especially for those whose daily activities or career depend heavily on sharp vision.
Common Treatments for CSC
There are several treatment options available depending on the severity and persistence of CSC. These may include laser photocoagulation, photodynamic therapy (PDT), and medications such as mineralocorticoid receptor antagonists.
Laser treatment is generally used when leakage points are identifiable and not too close to the central vision. Photodynamic therapy, which uses a light-activated drug to reduce choroidal vascular permeability, is often used in chronic cases.
Newer medical therapies, including oral medications, aim to reduce fluid build-up by targeting specific pathways involved in fluid regulation. While many patients respond well to treatment, it’s important to consider how vision might change over time following these interventions.
Short-Term Improvements vs Long-Term Outcomes
After CSC treatment, many patients experience noticeable improvements in visual acuity, color perception, and image clarity. In acute cases, vision may return to near-normal levels within a few months.
However, the long-term prognosis varies. Some individuals may continue to experience subtle distortions, decreased contrast sensitivity, or difficulties in low-light environments, even after fluid has been completely reabsorbed. These lingering symptoms can be frustrating, particularly if they affect the dominant eye or both eyes.
In chronic CSC, the prognosis becomes more complex. Repeated or prolonged fluid leakage can cause permanent damage to the retina, especially the photoreceptor cells. This may lead to lasting visual deficits even after treatment appears successful in stopping further leakage.
Risk of Recurrence and Vision Stability
One of the significant challenges with CSC is the risk of recurrence. Studies show that approximately 30–50% of patients may experience a recurrence after the initial episode. This is particularly common among individuals with chronic stress, ongoing corticosteroid use, or underlying health conditions that affect blood vessel function in the eye.
Each recurrence increases the likelihood of cumulative retinal damage, which may affect long-term vision prognosis. For patients undergoing central serous chorioretinopathy treatment, close follow-up with an ophthalmologist is essential to monitor for early signs of fluid reaccumulation. In some cases, preventative therapies or lifestyle changes may be recommended to reduce the risk of future episodes.
Lifestyle Adjustments and Monitoring
Aside from medical treatment, making lifestyle adjustments can also support long-term vision health. Managing stress, avoiding steroid medications where possible, and maintaining a healthy cardiovascular profile can help reduce the risk of CSC recurrence.
Regular eye check-ups are vital, even if vision seems stable. Advanced imaging techniques like optical coherence tomography (OCT) allow for precise monitoring of retinal changes, ensuring that any recurrence or residual damage is detected early.
Patients should also be aware that while vision can improve dramatically after treatment, it may not always return to pre-CSC levels, especially in chronic or untreated cases.
Conclusion
The long-term vision prognosis after central serous chorioretinopathy treatment is generally favorable for acute cases, with many patients regaining good visual function. However, chronic or recurrent cases carry a higher risk of residual vision changes and permanent retinal damage.
Being proactive about treatment, follow-ups, and lifestyle management significantly improves outcomes. For those undergoing central serous chorioretinopathy treatment, understanding the possibility of recurrence and the importance of retinal health monitoring can make all the difference in preserving vision over the years.